Iridectomy is a surgical procedure that is often performed for closed-angle glaucoma. Sometimes called peripheral iridectomy, the procedure involves removing parts of the iris and can be either invasive or less invasive. Less invasive iridectomy uses laser technology, while invasive iridectomy involves incisions.
In this article, we’ll answer some questions about the procedure as well as why it is performed.
What is the purpose of iridectomy?
Iridectomy is mainly performed to treat closed-angle glaucoma, which is a medical condition where the pressure inside your eye becomes too high than its normal pressure. Closed-angle glaucoma is much less common than open-angle glaucoma. In fact, around 90 percent of all glaucoma cases are open-angle glaucoma. People with closed-angle glaucoma experience pressure builds because fluid isn’t flowing around their eyes the way it should. This fluid is supposed to flow through the pupil into the front chamber of the eyeball, then goes through a series of channels known as the trabecular meshwork and into the veins of the white of your eye (sclera). This trabecular meshwork is damaged in closed-angle glaucoma, which makes it hard for the fluid to flow through the drainage pathway or even blocking the pathway completely. Because the fluid can’t flow through the drainage pathway, it backups and increases pressure inside the eyeball.
There are two types of closed-angle glaucoma: primary closed-angle glaucoma and secondary closed-angle glaucoma. In primary closed-angle glaucoma, your eye structures make it more likely for your iris (the colored circular membrane behind the cornea) to press against the trabecular meshwork, while in secondary closed-angle glaucoma, your eye experiences changes and forces the iris against the trabecular meshwork because of an underlying condition. These conditions include inflammation, tumor, diabetes, eye injury, and advanced cataract (clouding of the eye’s lens).
Numerous risk factors can increase the risk of developing closed-eye glaucoma. These risk factors include:
- Age. People who are older than 40, especially those between the age of 60 and 70 are more likely to develop closed-eye glaucoma.
- Farsightedness.
- Gender. Females are more prone to closed-eye glaucoma.
- Family history. If your family or siblings have this disease, your chance of developing the disease is a lot higher.
- Race. Southeast Asian and Alaska Native origins are a higher risk of developing closed-eye glaucoma.
There are two stages of this disease: acute and chronic. The signs of acute closed-angle glaucoma usually occur suddenly, such as severe eye pain, blurred vision, eye redness and tenderness, bright halos around objects, and nausea. The attack usually happens when the pupils are moderately dilated, such as when you are under stress or in a darkened room. Acute closed-angle glaucoma is an emergency condition and you need to call your local emergency number immediately. Chronic closed-angle glaucoma has subtler symptoms. Some people don’t notice any changes. Once the condition progress, you may experience deteriorating sight or losing the edges of your field of vision. Some people also experience redness and pain in their eyes, but not as severe as acute closed-angle glaucoma. Closed-angle glaucoma can result in optic nerve damage and vision loss.
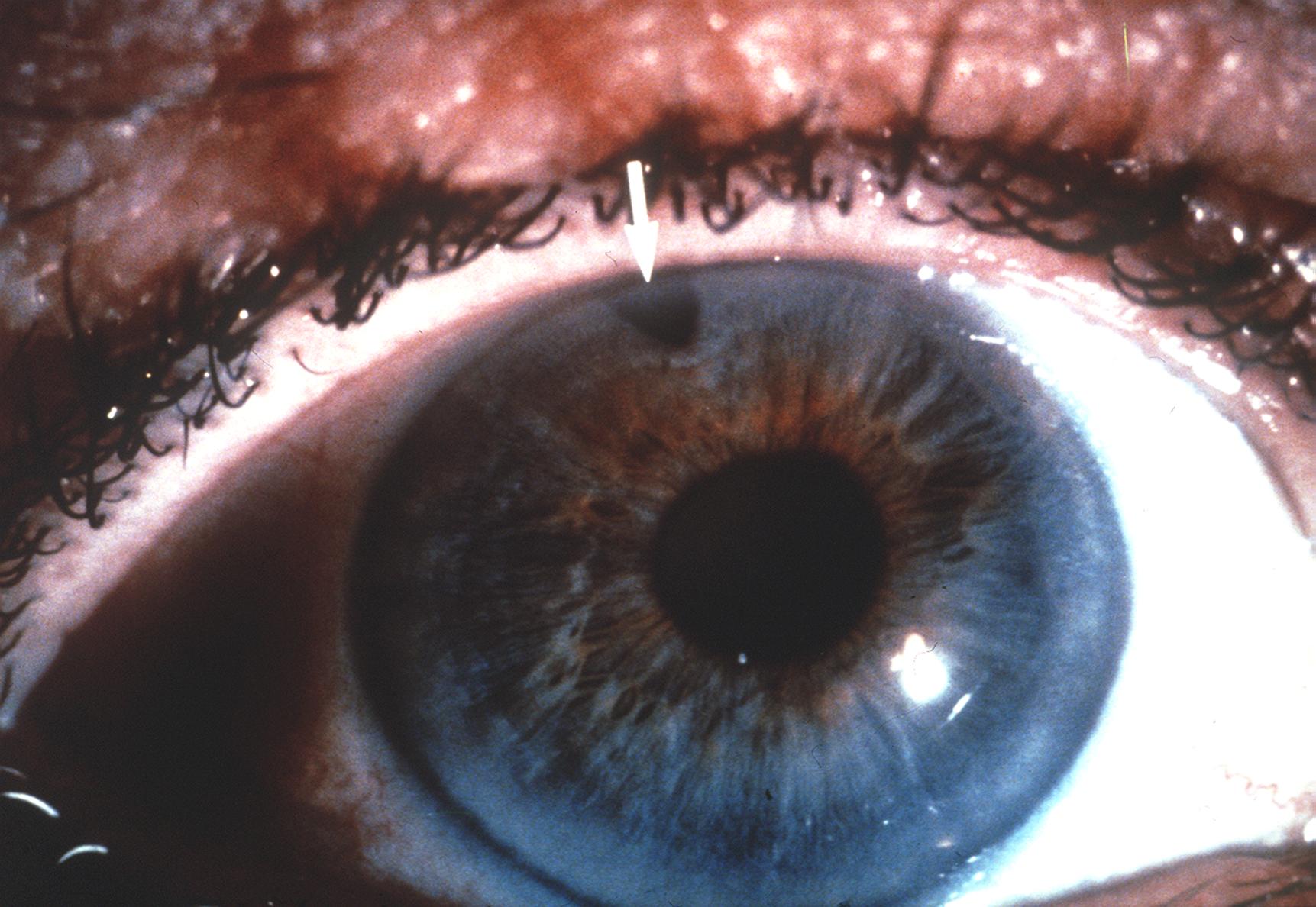
Although iridectomy is usually performed to treat closed-angle glaucoma, it can also treat melanoma of the iris. Melanoma of the iris is a malignant tumor that grows in the pigmented cells of the iris. This condition can enlarge and destroy your vision. It can also metastasize, spread other organs, and eventually cause death if left untreated.
How do I prepare for the procedure?
If you have a laser iridectomy, there are no special preparations. However, if you are scheduled to undergo a conventional iridectomy, you need to avoid eating or drinking for around eight hours before the procedure.
What happens during a laser iridectomy?
Half an hour before the procedure, your eyes are treated with drops to make the pupil small. You sit in a special chair and your chin has to rest on a frame to prevent your head from moving during the procedure. You are given anesthetic drops to numb the surface of the eye. A lens is placed on the eye to perform the lase, your surgeon uses a laser, usually an Nd:YAG laser, to create a hole in the outer edge of the iris, to relieve fluid pressure behind it. A full-thick section of your iris is removed. The procedure may take around 5 to 10 minutes and you may experience minor pain.
What happens during conventional iridectomy?
During conventional iridectomy, you lie on an operating table with a piece of sterile cloth around your eye. A general anesthetic is given to you before the procedure. Your surgeon uses special instruments to create incisions in the cornea and remove a section of your iris. The incision is self-healing and doesn’t require any stitches.
What to expect after the procedure?
You may experience temporary blurry vision and your eye may be sensitive to light, uncomfortable, and a little red. You may also experience a mild headache. The aftercare is minimal, but you need to strictly follow your surgeon’s instruction. Your surgeon may prescribe medication to help with your discomfort and headache, as well as eye drops to minimize the risk of infection. You will have to wear an eye patch for several days. Your vision will return to normal after six weeks, but you may go back to work the next day. After the procedure, you still need long-term medications to control the fluid pressure in your eye.
Is the procedure always successful?
Just like any other surgery, iridectomy is not always successful. However, the success rate is rather high. Around 60% of patients claimed that their conventional iridectomy is successful, while 15% said that their vision is better after the procedure.
What are the risks and side effects?
One of the risks of both conventional and laser iridectomy is that the angle may not open. When this happens, you may need further surgery. Other risks include infection, bleeding, scarring, and formation of cataracts. The side effect is irritation of the eye, which usually lasts for around two to three days.

